
Managing access to healthcare in Mozambique during the COVID-19 pandemic
Authors’ note: This work is being co-developed with Janeth Dula, Sergio Chicumbe and Eduardo Samo Gudo from the National Institute of Health at the Ministry of Health in Mozambique.
Low-cost solutions, like scheduled appointments, can improve healthcare delivery and medication adherence, while reducing vulnerability to infection.
The district hospital of Nicoadala in Zambézia province in Mozambique recently appeared in a mainstream newspaper outlet - O País - as a public health facility that was failing to implement the social distancing guidelines associated with COVID-19. According to the publication, “the volume of patients at the hospital was so great that they could not observe the stricture of no more than ten people gathering in one place, all under the gaze of the authorities responsible for the management of the hospital.”
 Source: O País, 9th April 2020
Source: O País, 9th April 2020
Congested and poorly managed health facilities
The Nicoadala facility is far from being an exception. Congestion in urban and peri-urban health facilities in sub-Saharan Africa has been extensively documented (Hardon et al., 2007; Yeap et al., 2010) with patients often spending several hours queueing to access a medical appointment or a pharmacy for medication.
Poor management of patient flows has been a long-standing problem in health systems in low and middle-income countries and one that can seriously compromise the quality of healthcare supply. Overstressed providers face menacing lines of disgruntled patients and often respond by shortening consultation times. Patients take queuing as a sign of an inefficient and disrespectful health system, which can reduce demand for healthcare and patient’s trust in medical advice. (Anderson et al., 2007; Hanefeld et al., 2017; Larson et al., 2018)
The Mozambiquan context:
- A high risk population
COVID-19 has brought renewed pressure for change in Mozambique. As the government moved quickly to reduce social contact, overcrowding in health facilities became a primary concern. Some of the groups considered to be under higher risk for severe illness by COVID-19 are also more likely to be queuing regularly at health facilities.
Patients with chronic diseases such as HIV, diabetes, and hypertension are often required to pay monthly visits to public health facilities for medication refills. These same patients may be at greater risk of developing severe disease if infected with COVID-19. HIV patients are among the groups that are most vulnerable to COVID-19 severity.
While it is to too early to know whether pregnant women and their neonates face increased risk due to COVID19, pregnant women, who have weakened immune systems and visit the health facility nearly monthly, may also be a cause for concern.
- Limited healthcare capacity: Equipment and personnel
Rapid transmission of the virus can have disastrous consequences in a context where the public health sector is systematically under-funded and already operating near capacity. There is a chronic lack of available beds in hospital intensive care units and very limited high-cost equipment for assisted breathing, such as ventilators (the last count in early April was 34 ventilators for a population of 30 million).
Moreover, the low number of medical personnel per capita means that should they become infected early on, there would be very limited capacity left to support a rising number of patients. In Mozambique, where foreign aid accounts for over 55% of the health sector budget (UNICEF, 2016), the physician-population ratio would have to be increased seven times in order to meet the World Health organisation’s (WHO) minimum recommendations.
- Waiting times and vulnerability to infection
As is the case in many low-income country settings, public health facilities in Mozambique follow a first-come first-serve model, where patients can only be seen by a provider if they arrive in the early hours of the morning, sometimes even before the centre is open.
Data from a study run by the International Growth Centre (IGC) (see further details below) in collaboration with the local Ministry of Health in 2017 showed that 66% of patients seeking antenatal care arrived at the facility before it even opened and that by 10 AM 94% of all patients had already arrived. Although queues started early in the day, patients spent several hours waiting before being seen. The average waiting time was over four hours for an appointment that would last, on average, 12 minutes.
Long waiting times can affect patients’ vulnerability to COVID-19 through two channels: First, queuing prolongs patients’ potential exposure to the virus while in clinic. Indirectly, if queuing leads to delays in medication adherence (because patients delay returning to health facilities they expect to be overcrowded, particularly in the context of requests for social distancing), this could weaken patients’ immune systems and potentially increase vulnerability to infection and severe disease.
- Medication adherence
In Mozambique, only 66% of HIV-AIDS patients who start treatment remain active after 12 months. This rate continues to drop in the following years, with retention rates of 49% at 36 months, a figure that is among the lowest in sub-Saharan Africa (UNAIDS, 2017).
Adherence to antiretroviral therapy (ART) is vital for HIV patients’ general health, reducing the chance of transmission and of ART resistance. It is also especially important in reducing vulnerability to COVID-19 (BHIVA, 2020). Moreover, while much remains to be learned about this particular coronavirus, past experiences with similar viruses suggest that immunocompromised patients may remain infectious for longer than other COVID-19 patients (CDC, 2020).
Pilot intervention: Scheduled appointments
The IGC and the Mozambican Ministry of Health are currently testing the impact of a scheduling system that allocates specific timeslots for appointments in HIV and prenatal care in public health clinics in Southern Mozambique in a randomised controlled trial (RCT). The system aims to improve the allocation of patients across times of the day and days of the week to facilitate patients being seen within one hour of their arrival. This RCT is taking place in 72 high-volume public health facilities in urban and peri urban areas, serving over 266,400 patients.
The main goal of the scheduling intervention is to significantly reduce waiting times for patients, thus improving patients’ experience and reducing the opportunity cost of attending prenatal consultations and ART therapy (seeking clinical care and taking ART refills). Importantly, controlling access and time in clinic is critical to ensure that public health facilities do not become foci of contagion during the pandemic.
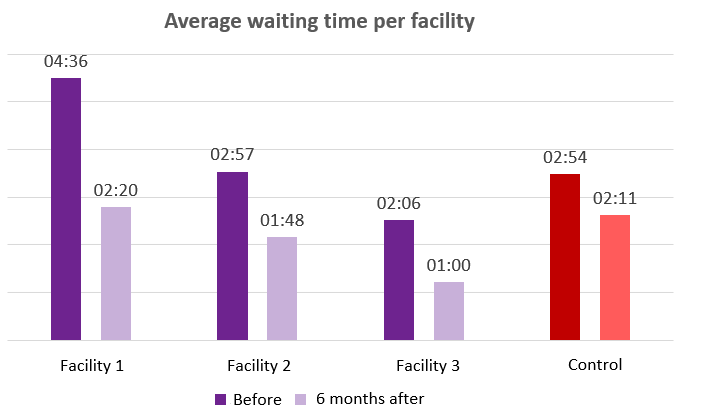
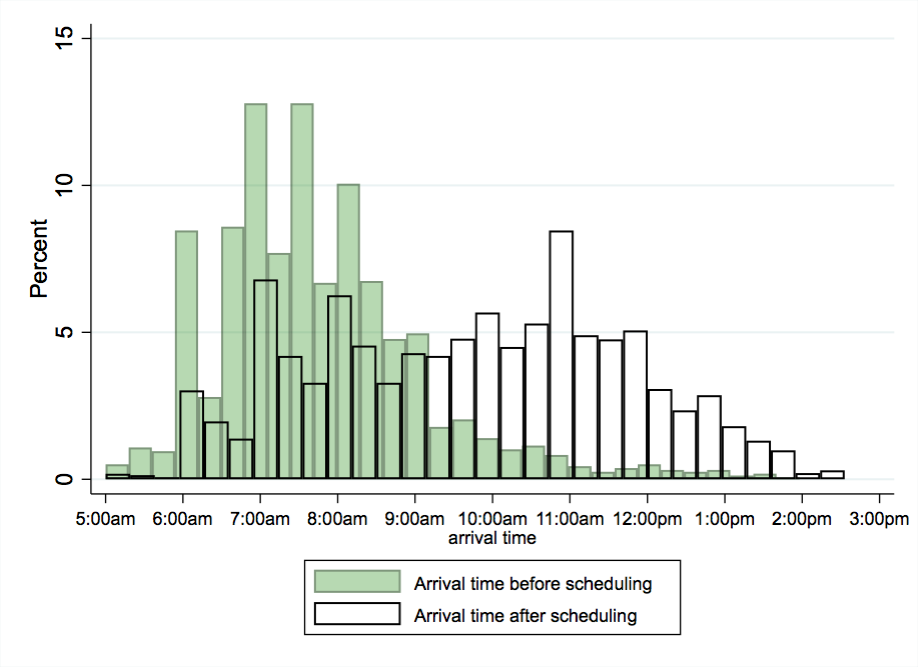
A successful pilot in three clinics revealed that a scheduling intervention reduced waiting times by approximately 50% (see Graph 1 below). Patients began to arrive, on average, 12 minutes before their consultations and only 7% of them arrived after the scheduled time, indicating that a shift in norms and adherence to the new system is possible (see Graph 2). Interviews with over 1,600 patients revealed that the vast majority (almost 99%) were highly satisfied with the system of scheduling appointments.
Graph 1: Waiting times in treatment and control facilities in pilot study
Graph 2: Arrival times with and without scheduling
Conclusion: Low-cost interventions with impact
Moments of crisis can provide the impetus for long-lasting change. Low-cost, low-tech solutions to problems of frontline management in clinics have the potential to offer an opportunity for meaningful improvement at scale in the way care is delivered in low-income countries.
Introducing scheduling systems and managing patients’ interactions in clinics might prove to be a critical tool for health systems to navigate, and survive, the COVID-19 pandemic. Additionally, this will improve the long-run capacity of the health system to deal with likely increases in demand in the future.
Disclaimer: The views expressed in this post are those of the authors based on their experience and on prior research and do not necessarily reflect the views of the IGC.

