
Vaccine uptake and resistance: Lessons and policy levers
As new variants of COVID-19 are disrupting global efforts to end the pandemic, governments need to work faster to immunise populations and curtail the spread. This blog examines lessons and policy solutions for global immunisation efforts, drawing from recent evidence on vaccine acceptance in low- and middle-income countries.
With the urge to vaccinate their populations mounting, high-income countries began driving their health systems towards aggressive mass vaccination campaigns just under a year since the start of the pandemic. As of July 2021, vaccination has lagged behind in most low- and middle-income countries (LMICs), as supply chains for the vaccines have only recently begun to emerge. A mere 1.1% of the population in low-income countries have been given at least one dose of the vaccine, while more than 1 out of 4 have received it in the rest of the world. Most of the successful vaccine candidates are manufactured in high-income countries, with their transportation relying on sophisticated procedures. To address challenges to vaccine access, the WHO is directing the COVAX initiative, aimed at delivering 1.8 billion doses across 92 low-income countries by early 2022.
Willingness to vaccinate against COVID-19 in LMICs
In a survey spanning more than 22,000 individuals in 10 LMICs, researchers from the IGC and over 30 partner institutions, including Innovations for Poverty Action (IPA), WZB Berlin Social Science Center, the Yale Institute for Global Health, and the Yale Research Initiative on Innovation and Scale (Y-RISE), assessed willingness to vaccinate against COVID-19 in LMICs. Our study, recently published in Nature Medicine, points to significantly higher vaccine acceptance in LMICs as compared to the acceptance rate in Russia and the US, and healthcare workers being considered the most trusted for information on vaccines. These and other findings have important policy implications for the design and implementation of effective vaccination campaigns in LMICs. Importantly, they show that prioritising the distribution of vaccines to LMICs should yield high returns in expanding global immunisation coverage.
Vaccination campaigns in LMICs – currently focused predominantly on childhood vaccines – are needed for adult vaccines on an unprecedented scale. Recommended adult vaccines like the seasonal influenza vaccine are underused in LMICs: as of 2014, only 1 in 3 LMICs had a vaccination programme for influenza.
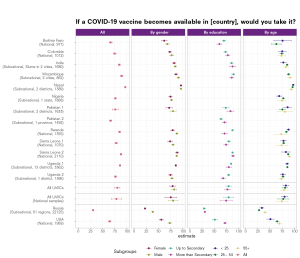
The surveys gather data from Burkina Faso, Colombia, India, Mozambique, Nepal, Nigeria, Pakistan, Rwanda, Sierra Leone, and Uganda. As reference points, we also include data from around 24,000 respondents in Russia and the US. The data was collected through a combination of phone and internet surveys by IPA, the IGC, and WZB. It is worth noting that the data is not fully representative, and for some countries (India, Mozambique, Nepal, Nigeria, Pakistan, Russia, and Uganda), our study covers only sub-regions. Caution should therefore be used in extrapolating the results highlighted in the study.
Acceptance rates are sufficient to reach immunisation thresholds in LMICs
Our study reveals encouraging findings on the level of vaccine acceptance in LMICs. With an average acceptance rate across surveys of around 80%, ranging from 67% in Burkina Faso to 97% in Nepal, predicted uptake would be above the required herd immunity threshold (60-70% according to most estimates). This is significantly higher than in Russia (30%) and the US (60%). This varies also slightly within each country across different socio-demographic groups, with women for instance tending to be less willing to take COVID-19 vaccines. Their acceptance rate across LMICs is, on average, 4.2 points below that of men.
Figure 1: Acceptance rates, overall and by respondent characteristics
Motivations behind vaccine uptake/refusal
Respondents who said they were willing to get vaccinated were asked about their motivation for uptake. Personal protection is the main reason given for vaccine acceptance, distantly followed by family protection. Community protection was consistently mentioned by less than 1 out of 4 respondents within each of the LMICs surveyed. This is an important takeaway informing early debates on immunisation, which tended to focus on altruistic attitudes towards community protection. Interestingly, this personal motive is also highlighted as one of the reasons for vaccine refusal, with a majority of respondents who are not willing to get the vaccine mentioning concerns about its side effects.
The discrepancy between the proportion that are generally pro-vaccination and the predicted uptake for the COVID-19 vaccines shows that the profile of those refusing the COVID-19 vaccine is not the profile of the typical anti-vaxxer. Additionally, few respondents cited conspiracy theories as reason to refuse a COVID-19 vaccine.
Policy levers: Cash transfers, messaging, and social signalling
Despite the level of vaccine acceptance being high enough for mass immunisation, there is room for improvement, even in those countries with the highest vaccine acceptance. Last-mile nudges as they are used for other vaccines could prove effective to maximise uptake. The goal to eradicate childhood diseases such as measles and polio led to global and systematic efforts to bring vaccination rates, that were around 90%, to the needed threshold of 95%. In Nicaragua, cash transfers conditional on healthcare appointment attendance (during which vaccination was realised as part of the ‘Red de Proteccion Social’ programme) led to a 23 percentage points increase in on-time and full vaccination coverage of children aged 12-23 months. Interestingly, this increase was even greater for populations traditionally difficult to target, like children with less educated mothers or whose homes are further away from health centres.
Recent research has also found messaging can improve vaccination attitudes. An experiment by Alatas et al. (2019) in Indonesia found that a message on immunisation was, on average, 1.7 times more likely to be retweeted or liked when it was shared by a celebrity as compared to a regular user. Additionally, this online effect translated into an offline effect: commonly believed myths such as "vaccines are not halal", "vaccines can be substituted with natural alternatives", or "mild side effects should be an alarm on the safety of the vaccine" were given less attention following exposure to Twitter content promoting immunisation.
Figure 2: Most trusted source for COVID-19 vaccine decision making (developing country respondents)
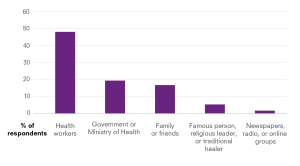
Our study shows that healthcare workers are consistently cited as the most trustworthy source of information on COVID-19 vaccines, far ahead of celebrities and religious leaders, except in Rwanda where the government is a more trusted source. Respondents also named friends and family as trustworthy sources of information.
In fact, some studies have examined the role of social signalling in increasing immunisation. For example, a field experiment in Sierra Leone by Anne Karing introduced a simple way for parents to signal that they had vaccinated their children by wearing a coloured bracelet (a signal of responsibility). Parents sought out this community-wide social signalling and as a result, childhood immunisation increased.
To note, the data in our study was collected at a given point in time, in the fast-moving context of the pandemic. Some survey data was collected prior to the first announcement of a vaccine candidate concluding phase III of testing. These surveys could therefore underestimate the real vaccine acceptance rate in these countries. Additionally, stated acceptance of the vaccine might not necessarily translate into actual uptake – highlighting a crucial policy concern for LMICs. The vaccine acceptance estimates provided by our study should serve as a reference point for future efforts by health authorities to continue monitoring vaccine acceptance.
Living with the virus
As Hans Heesterbeek, Professor of Theoretical Epidemiology at Utrecht University, suggests: “There is little reason to believe that the coronavirus SARS-CoV-2 will go away any time soon, even when vaccines become available.”
COVID-19 will not disappear as soon as the mass immunisation threshold is reached. It is more likely a permanent virus that most countries will need to learn to live with. The fact that most developed vaccines require two doses poses an endorsement challenge in itself. New variants will motivate new vaccines and new vaccination campaigns may be needed. The supply of COVID-19 vaccines remains a major concern, with a multitude of hurdles for mass distribution – from storage requirements for shipping to the speed of manufacture. While our study provides some insights into vaccine acceptance in LMICs, the demand-side challenges are huge and complex in both high- and low-income countries, and most importantly, will not necessarily be mitigated with time. Policymakers will have to continue to concerted efforts to address vaccine hesitancy nimbly and flexibly, drawing from academic evidence that is emerging and lessons from other countries.

