
What happens after the lockdown ends? Lessons from the 2015 Ebola epidemic in Sierra Leone
There have now been over 5 million confirmed cases of COVID-19 around the world, with the number of deaths moving towards 350,000. Policymakers in many countries have responded to the pandemic by implementing measures related to social distancing and a large share of humanity remains in some form of lockdown condition. As a consequence of the uncertainty caused by the pandemic, economic activity has contracted, hitting hardest firms and workers whose activities rely on face-to-face contacts.
Low income countries with weaker health infrastructures, lower state capacity, and greater paucity of data to inform policy face an even tougher challenge between health and economic costs. The need to balance these challenges during the crisis has been much discussed, but an equally important aspect to think through is the potentially longer lasting impacts of policies used now to tackle the pandemic. While the immediate costs of the crisis are large and visible, long-run consequences are less visible but potentially larger.
In this article, we consider what we might learn from the last time developing countries faced similar twin health and economic challenges: the 2014-16 Ebola epidemic in West Africa. This represented the, "longest, largest, deadliest, and...most complex [Ebola outbreak] in history.” We consider two central policy responses: market closures and school closures. We particularly focus on the potential impacts of these two policy responses on young women, using the findings from our own study to highlight these consequences and potentially motivate interventions to counter these adverse impacts.
The timeline of the Ebola epidemic and policy responses
The 2014-16 Ebola outbreak affected Sierra Leone, Guinea, and Liberia, and infected close to 30,000 individuals, killing over 11,000. Sierra Leone was the most affected country, hosting half of all cases. Figure 1 charts the timeline of the epidemic in Sierra Leone. This shows how rapidly Ebola spread: within months of the first recorded case in May 2014, the virus had spread to all 14 districts in the country. The peak flow of weekly cases occurred in December 2014. It took until July 2015 for the flow of new cases to finally get closer to zero, and Sierra Leone was declared Ebola free in November 2016.
The epidemic had severe consequences for the healthcare infrastructure that was already among the weakest in sub-Saharan Africa. Ebola caused the death of many health workers and eroded public trust in using health facilities even further. The collapse of the healthcare system meant access to standard medical services, such as antenatal and maternal care, was severely hampered during the outbreak. A combination of capacity constraints and fear of hospitals led to considerably fewer women accessing antenatal care or giving birth in health facilities during the crisis.
Figure 1: Timeline of the Ebola epidemic in Sierra Leone
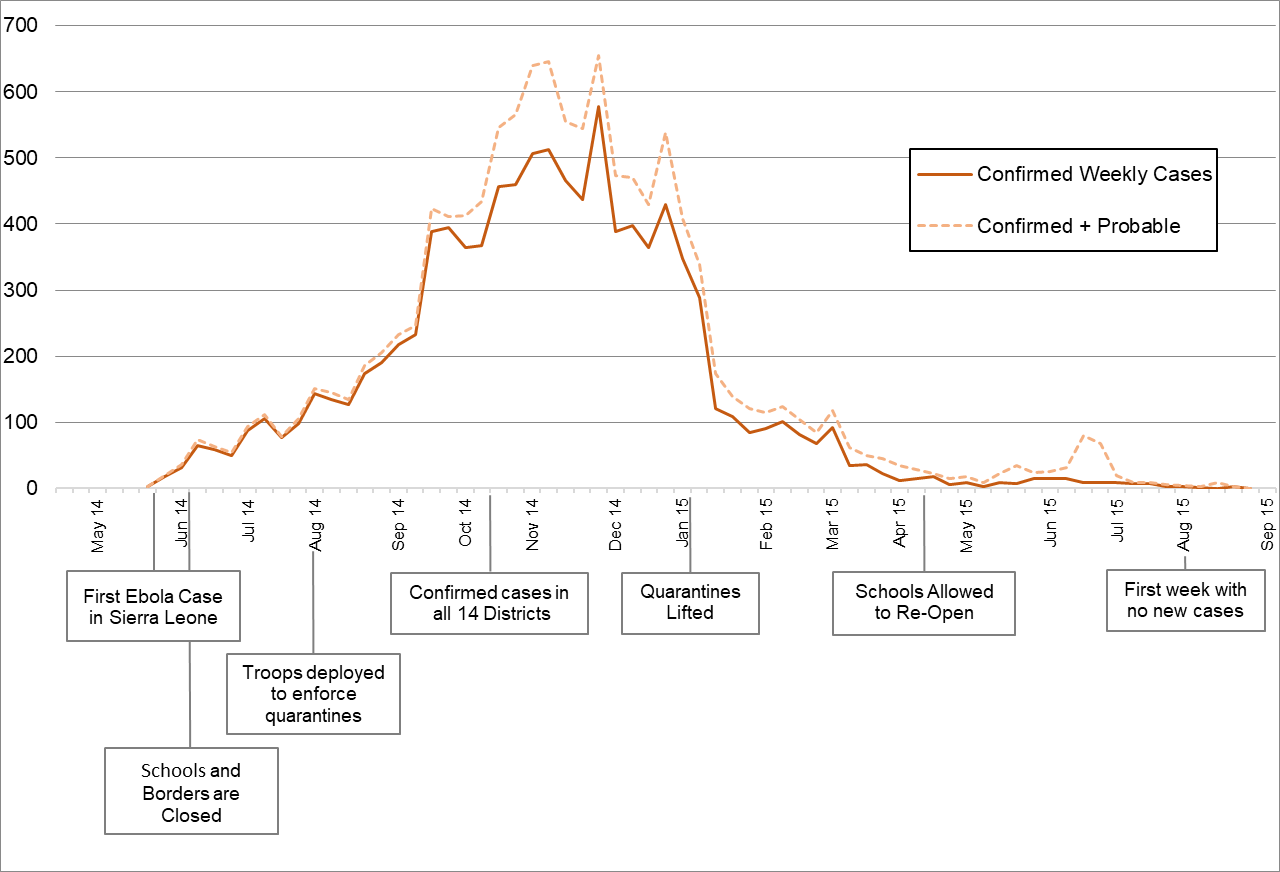
The lower part of Figure 1 shows the timeline of the two main policy responses we focus on here: (i) communities were locked-down, markets closed, and travel bans introduced; (ii) all primary and secondary schools were closed through the 2014-15 academic year.
Similar policy responses of limiting mobility, and market and school closures have been used to a large extent in the current crisis. This has again been driven by the need to limit human-to-human transmission of COVID-19 through social distancing (although Ebola is transmitted mostly through bodily fluid, while COVID-19 appears far easier to transmit through near contact). For example, schools have been closed in 153 countries, affecting close to 1.2 billion children. We consider how economic activity recovered in Sierra Leone and some of the long-term repercussions of school closures, while trying to highlight suggestive implications for how countries might tackle the current crisis.
Lesson 1: Economic crisis and a slow recovery
The economic impacts of Ebola during the epidemic in Sierra Leone were enormous: in a year, the annual growth rate of GDP plummeted from 8.9% to -2.0%. Market closures impacted those whose livelihood depended on them. The self-employment sector, which accounted for 91% of the labour force, shed around 170,000 jobs (with revenues for surviving enterprises falling by 40%), and a further 9,000 jobs were lost in wage employment.
The crisis impacted economic opportunities for all. However, women might have been relatively more impacted by the economic disruption because women’s labour force participation rates are higher than men up until age 30. While agriculture is the main source of employment for both men and women in Sierra Leone, young women are particularly reliant on self-employment.
To see patterns of post-epidemic recovery after restrictions on mobility and markets were lifted, Figure 2 shows the time series for GDP per capita in Sierra Leone. Pre-epidemic Sierra Leone was enjoying rapid growth, especially given a surge in growth from 2011, and international predictions were for this to be sustained over the coming years. Then Ebola struck. Over the course of epidemic GDP per capita fell by 22%, going back to its level in 2012. Starting from 2016, there was a gradual recovery in economic output, but even by 2018, GDP per capita had risen by only 13% and was still far below its pre-crisis level. It essentially appears to have returned to its pre-2011 trend. This speed of recovery is slower than that from other macroeconomic crisis such as conflict, but perhaps not as slow as recoveries documented in the aftermath of political or financial crises.
Figure 2: GDP per capita in Sierra Leone
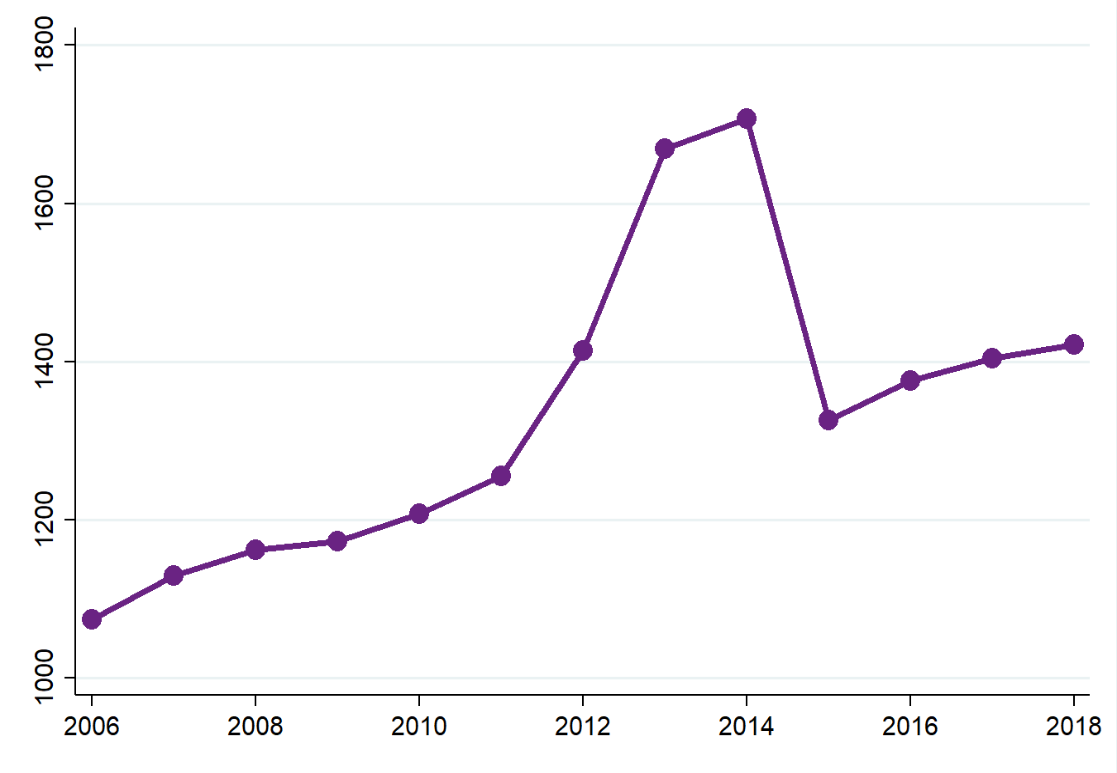 Source: World Development Indicators
Source: World Development Indicators
It is too early to tell to what extent West African countries will be impacted by COVID-19 in terms of the number of cases and deaths from the virus. Africa, as a whole, currently has close to 111,000 confirmed cases, with more than 3,300 deaths. Nevertheless, perhaps because of recent experiences with Ebola, they have implemented similar policies of social distancing quickly (even before many cases had been confirmed), and this might lead to a similar path of economic shock and recovery as with the Ebola epidemic. At the same time, the current crisis is global and has shut down many international supply chains, while the Ebola epidemic only affected Sierra Leone and its neighbours in West Africa.
Lesson 2: The persistent effect of school closures
As part of social distancing measures to prevent contagion during the Ebola epidemic, schools were closed in May 2014 and re-opened in April 2015 as the epidemic began to slow (the school year runs from September to July). Most students lost around 39 weeks of schooling as a result. Moreover, just before schools were due to re-open in April 2015, the Ministry of Education, Science and Technology announced the continuation of a pre-Ebola policy that disallowed “visibly pregnant girls” from re-enrolling.
This policy response had particularly acute impacts on young women. Without the protection of time in school:
(a) young girls may spend more time with men and face increased risks of getting pregnant, which will then adversely affect their education because they would not be allowed to re-enrol in school if visibly pregnant, and because of the adverse impacts of early motherhood on labour market outcomes;
(b) young women then become more vulnerable to sexual abuse, limiting their ability to accumulate human capital in future.
This raises the possibility that even temporary school closures could have very persistent impacts on the lives of some young women.
Analysing the effect of safe spaces for women during the Ebola epidemic
Our data collection exercise in Sierra Leone was originally planned to evaluate an intervention to empower young women, building on our earlier work evaluating the same intervention in Uganda. The programme, known as the Empowerment and Livelihood for Adolescents (ELA) intervention, is delivered by the NGO BRAC. It provides clubs in which young women can meet, offering them a package of vocational skills training, financial literacy, and information on health and reproductive issues. Most importantly, the ELA clubs offer women a safe space to meet.
Fieldwork for our baseline was completed a week prior to the first cases of Ebola being reported in May 2014. In our follow up survey in early 2016, we were able to track 4800 girls in 200 villages across four districts. We use this survey data to measure how the Ebola shock impacted their lives, assessing the lasting impacts post-epidemic, when lockdown policies had ended, and markets and schools had reopened. We exploit the randomised roll out of the ELA programme to understand whether the safe spaces established as part of the ELA intervention prior to the epidemic mitigated any of these impacts.
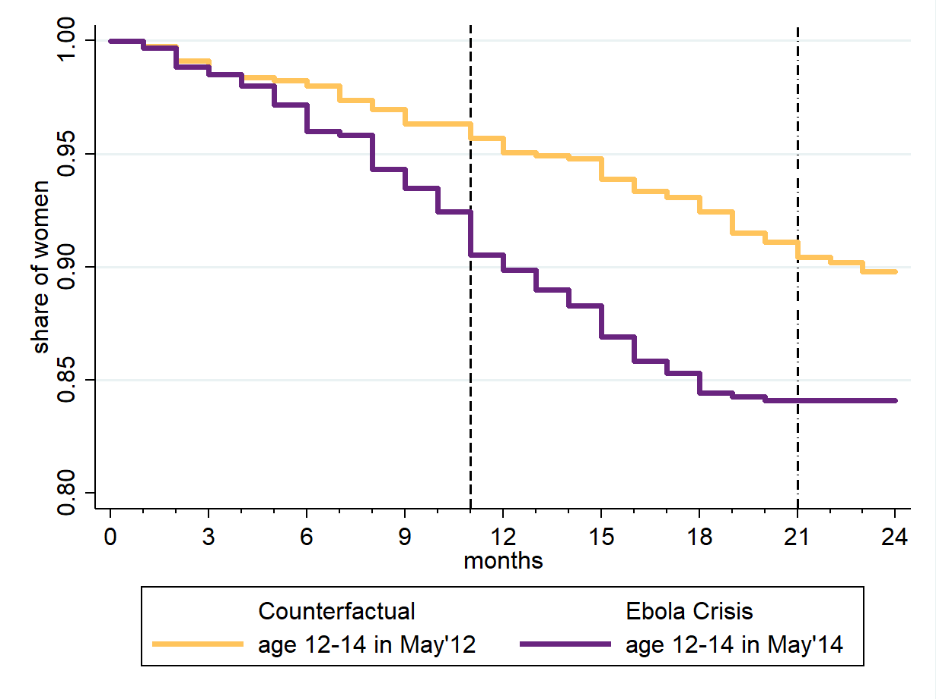
Figure 3 highlights how the Ebola epidemic increased the vulnerability of young girls, as measured by the likelihood they became pregnant during the crisis. The horizontal axis represents time, in months, from either May 2014 (the start of the epidemic) or May 2012 (the start of our pre-epidemic counterfactual period). At time zero, each sample includes only young women age 12-14 in the reference year that have never been pregnant. The vertical axis measures the share of young women in each sample that become pregnant over time: either in the two years before the epidemic, or the two years during the epidemic.
We first focus on those in control villages, girls that were never offered the safe space of the ELA clubs. We see that relative to the pre-Ebola counterfactual, pregnancy rates increase dramatically for these young girls. In the two years pre-epidemic, 10% of these girls became pregnant. In the two-year window of the crisis this rises by nearly half again, with around 15% of girls becoming pregnant. These pregnancies are conceived evenly over the crisis: starting from May 2014, the first vertical dashed line shows when schools started to reopen and the second shows when Sierra Leone was finally declared Ebola free.
Figure 3: Time to first pregnancy, Control group
 Women without Children at Month=0
Women without Children at Month=0
Our formal analysis more precisely shows that over the course of the Ebola epidemic, out-of-wedlock pregnancy rates for girls aged 12-17 at the onset of the crisis, increased by 7.2 percentage points. However, this was entirely reversed for those that had access, prior to the epidemic, to the safe space of an ELA club in the most highly disrupted treated villages. The changes in pregnancy then map closely back to school enrolment post-crisis, and thus have important implications for the ability of these young girls to raise their human capital in the long-run. In control villages, school enrolment rates fell by 16 percentage points over the crisis, but this was halved in the most disrupted treated villages. This was largely a result of young girls not becoming pregnant during the crisis and thus being able to re-enrol when schools reopened. Using further data from our surveys, we are able to pinpoint some of the key changes in the lives of young women. We find that girls with prior access to ELA clubs report spending much less time with men, and are able to retain more of their social ties to others post-epidemic.
Implications for COVID-19
The World Bank’s recent Africa Pulse report projects the current crisis will push sub-Saharan Africa into recession in 2020, potentially costing the region up to $70 billion in lost output. Recent history shows us that the economic and social recovery from the Ebola epidemic was slow for Sierra Leone. Beyond the national level, the evidence also indicates that the Ebola epidemic may have impacted people in different ways and in particular changed the life trajectory of many adolescent girls. Temporary school closures and the lack of economic opportunities drove them to spend time with men, which resulted in increased early childbearing and permanently dropping out of education. Some of the long-run costs of the epidemic are going to be through this channel of lost human capital accumulation of young girls.
Of course, during the current epidemic schools have to be closed. However, the policy that prevented visibly pregnant girls from re-enrolling in school post-epidemic was especially harmful. This needs to be considered when lockdown policies eventually come to be reversed, as other countries have implemented similar restrictions on the re-enrolment of pregnant girls. Even without formal restrictions, however, pregnant girls may require additional forms of support to overcome informal barriers, such as stigma or care responsibilities, to re-enrol once school closures are lifted.
What further lessons will be relevant for the COVID-19 pandemic? Clearly, any policy response needs to adhere to social distancing, so alternative safe space provisions need to be thought through. For example, interventions supporting young women through virtual mentoring or phone-based group chats, or any form of feasible group activities. These might go a long way in making sure that a short-lived epidemic shock does not damage lives in the long-run. Such activities can also help girls build and maintain their social networks, therefore enabling them to be more resilient during the crisis. They can also enhance a more rapid recovery because with poorly functioning markets, having access to informal credit and advice through social ties is especially important for the speed of economic recovery.
Our evaluation also suggests that equipping young women with a minimal set of competencies on reproductive health – such as using contraceptives - during the crisis might go a long way to protecting their welfare in the longer term. The importance of addressing these challenges is clear: many countries throughout sub-Saharan Africa have relatively young populations (and thus actually relatively fewer older people more susceptible to COVID-19), and so school closures could leave many adolescent girls vulnerable. Acting now and with thought for the dynamic effects of policies, can positively affect lives now and in the future.
Editor’s note: A version of this article first appeared on The Conversation.
Disclaimer: The views expressed in this post are those of the authors based on their experience and on prior research and do not necessarily reflect the views of the IGC.

