
Timeliness and coverage of child vaccinations across India
Despite free vaccinations for children below 12 years of age under the Universal Immunisation Programme, one-third of global child deaths due to vaccine-preventable diseases occur in India. In this article, Debnath and Chaudhuri use nationally representative data from 2005-06 and 2015-16, to examine the timeliness and coverage of routine immunisation in the country. Further, they discuss findings from a recent primary survey in Bihar to gauge the impact of COVID-19 in this regard.
Despite a significant increase in immunisation coverage in India, about two-thirds of all types of deaths in children aged below five years of age are due to diseases that can be prevented by vaccines. A major underlying factor behind these deaths is delay in vaccination (Liu et al. 2016). In addition, studies on vaccination timeliness suffer from measurement error due to missing and incorrect variables, limitations of record-based data, and lack of scale.
Under the Universal Immunisation Programme (UIP), immunisation in India is provided free of cost against 12 vaccine-preventable diseases.[1] Despite more than three decades of the UIP, one-third of global child deaths due to vaccine-preventable diseases occur in India (Black et al. 2010), and India also constitutes the largest share among unvaccinated children in the world (Centers for Disease Control and Prevention (CDC), 2013). According to India’s National Family and Health Survey (NFHS)-4 (2015-16), only 62% of all children between the ages of 12 and 23 months have been administered all basic vaccines.[2]
Why timing matters
The appropriate age for vaccines depends on when maternal antibodies cease to provide protection, and the earliest age at which vaccinations can be safely administered with maximum efficacy. Delayed vaccination causes children to have little immunity when they are most vulnerable to diseases. This is also known to disturb the development of ‘herd immunity’ [3] (Guerra 2007). For instance, unvaccinated older siblings can act as vectors of whooping cough for their younger siblings (Izurieta et al. 1996). Furthermore, a delay in vaccinations that are meant to be given to children at early stages, is correlated with delays in subsequent vaccinations (Kiely et al. 2018). Often, a subsequent vaccine is bundled with the delayed vaccine, which may mean that the latter is delivered prematurely. Evidence shows that premature measles vaccines have reduced efficacy since these are neutralised by maternal antibodies. Also, the bundling of measles and DPT-3 vaccines leads to complications and a proportionately higher mortality rate among girls as a side effect of the concoction in administration (Awofeso et al. 2013).
Pathways causing delays
Vaccinations in rural India are delivered by auxillary nurse-midwives (ANMs) who are assisted by ASHAs (Accredited Social Health Activists) [4] at the village level. ANMs are government employees whose salaries are independent of their performance, while ASHAs are paid according to fee-for-service. One of the primary responsibilities of ANM and ASHA workers is to organise Village Health and Nutrition Days (VHND), where – among other health, nutrition, and sanitation services – infants are vaccinated. The responsibility to prepare for these sessions rests with ANMs, who comb through birth records of recently born infants in their jurisdiction and create a list of those due for vaccination. However, such large-scale collection and organisation of critical primary data is labour-intensive and leaves a significant margin for human error. These lists tend to reach ASHAs from ANMs on or the day before the VHND session, making it difficult to mobilise those due for their vaccines. Furthermore, dealing with large amounts of paperwork often reduces the time available for service delivery.
On the demand side, parental decisions play a pivotal role – socioeconomic factors, lack of awareness, and religious beliefs are all documented factors behind vaccine delays (Mathew 2012, Choudhary et al. 2019, Pati et al. 2011). Choudhary et al. (2019) focus on the predictors of delay in BCG, DPT-1, and measles vaccination. Children born through home births are 2.7 times more likely to have a delay in BCG vaccination (Tauil et al.2016). Parental concerns over the safety and benefits of vaccination play a role in the delay of vaccination for infants with low birth weight (O’Leary et al. 2016). Evidence also shows that the higher the birth order, the higher the chances of a delay in age-appropriate immunisation. Early age at marriage and lower maternal education predict delay in vaccinations, most likely due to lower awareness and receptiveness to health messages (Mathew 2012, Pati et al. 2011). Economically weaker sections of the society also fare worse, owing to a lack of awareness and utilisation, and social, financial, and physical barriers to access (Awofeso et al.2013, Mathew 2012).
Timeliness in immunisations for children
We use NFHS-4 (2015-16) data to study average district-level timeliness in immunisations for children under five years of age. To highlight the spatial distribution of timeliness, we plot the statistics for BCG and DPT-3/Pentavalent-3 [5] vaccines.
Figure 1. District-wise timely administration of BCG vaccine
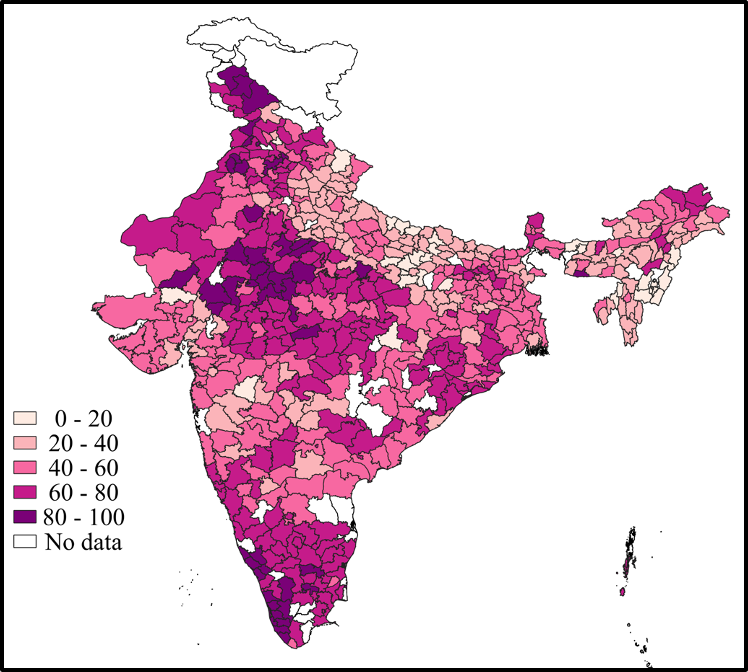
Source: NFHS-4
Note: (i) The figure plots the percentage of infants under five years of age who received the vaccine on time. (ii) We consider a vaccine to be timely if it is administered within seven days of the date it is due.
Figure 2. District-wise timely administration of DPT-3/Pentavalent vaccines
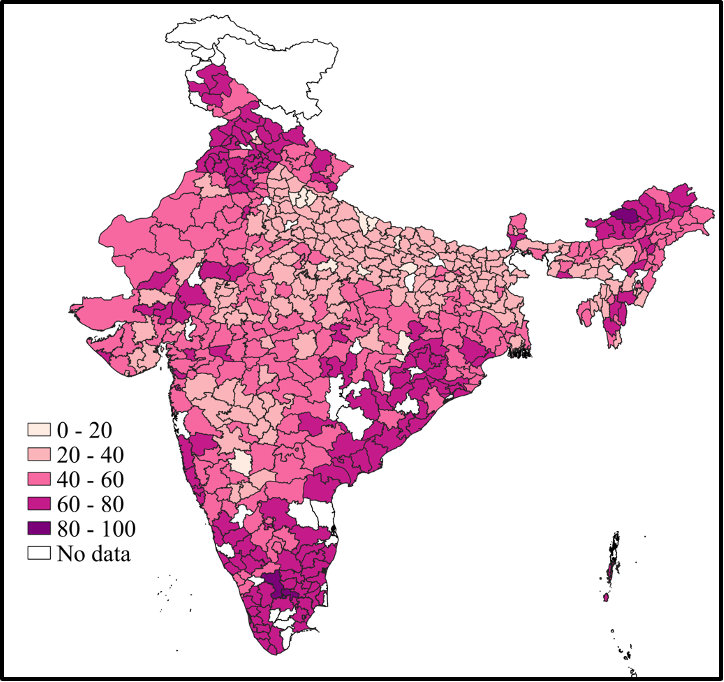
Source: NFHS-4
Note: (i) The figure plots the percentage of infants under five years of age who received the vaccine on time. (ii) We consider a vaccine timely if it is administered within seven days of the due date.
As expected, the figures show that BCG, administered at birth, is more often delivered on time than DPT-3, which is to be administered 14 weeks after birth. Besides, there is substantial geographic variation in the timeliness of the delivery of these vaccines, with some districts in Bihar, Madhya Pradesh, Maharashtra, Uttar Pradesh, and parts of Northeast India underperforming.
To understand the change over time in immunisation of children below five years of age in India, we report coverage and timeliness in administering several vaccines from two subsequent rounds of the NFHS (NFHS-3 (2005-2006) and NFHS-4 (2015-2016)) in Table 2.
Table 2. Vaccine coverage and timeliness
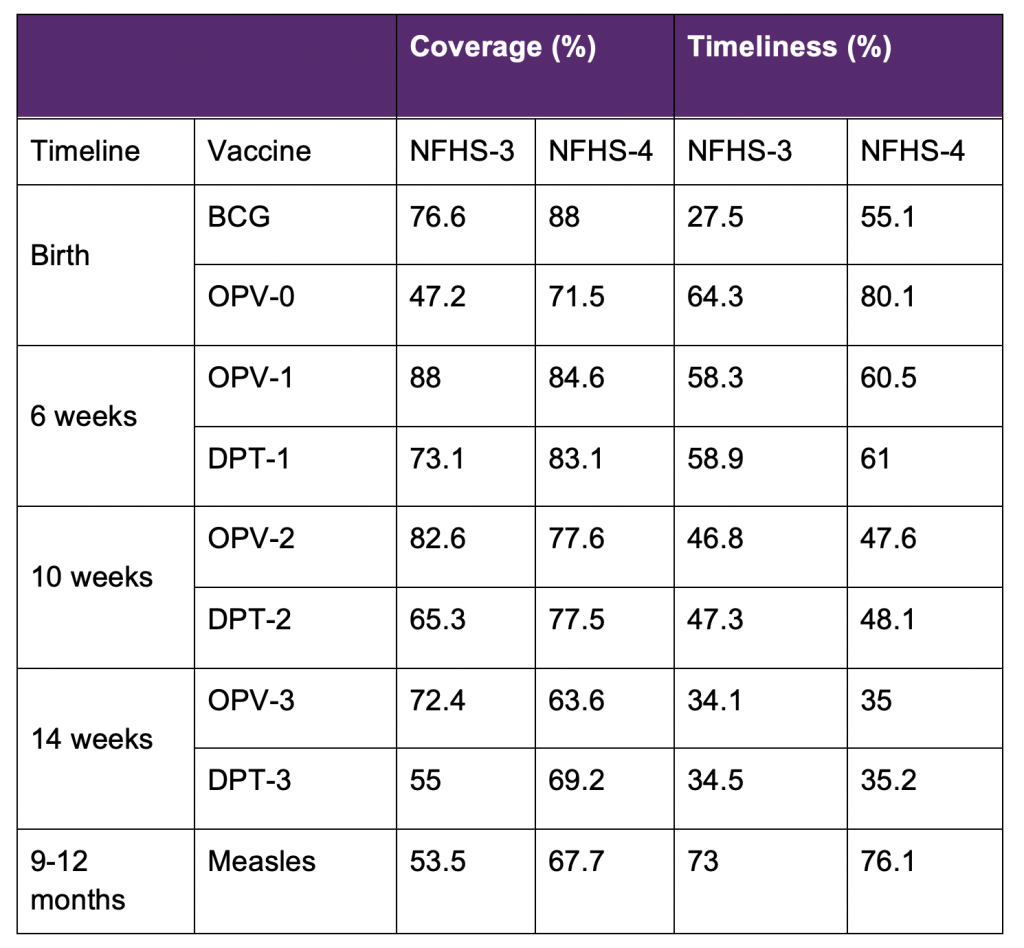
Source: NFHS-3, NFHS-4.
Notes: (i) We consider children below five years to calculate coverage and timeliness. (ii) We consider a child as vaccinated if the primary caregiver reports that the child was vaccinated or the MCP (mother-child protection) card records vaccination. [6](iii) To calculate timeliness, we consider children with a valid date of vaccination on their MCP cards. (iv) OPV stands for oral polio vaccine.
The coverage for most vaccines we study shows a substantial improvement in the 10-year period between the two rounds of NFHS data. Overall, we find that the coverage and timeliness of vaccines administered at birth are substantially better than the booster doses. However, coverage of the booster doses of OPV declines over time, and there is also no discernible improvement in their timeliness. Despite being easier to administer, a declining trend in the coverage of OPVs must be a concern for health policymakers. The timeliness of vaccines other than BCG and OPV-0 do not show any considerable improvement over these 10 years.
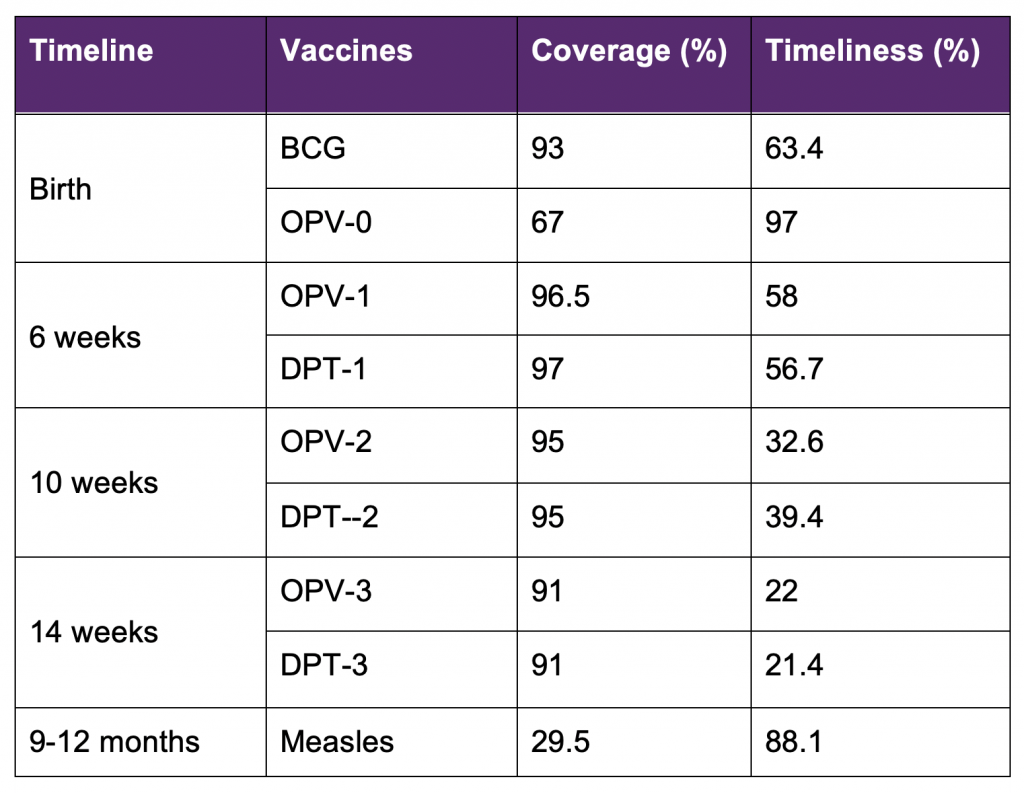
We plot the cumulative percentage of infants receiving BCG and DPT-3/Pentavalent-3 vaccines as they become older in Figures 3 and 4 below.
Figure 3. Change in timeliness of BCG vaccine for infants
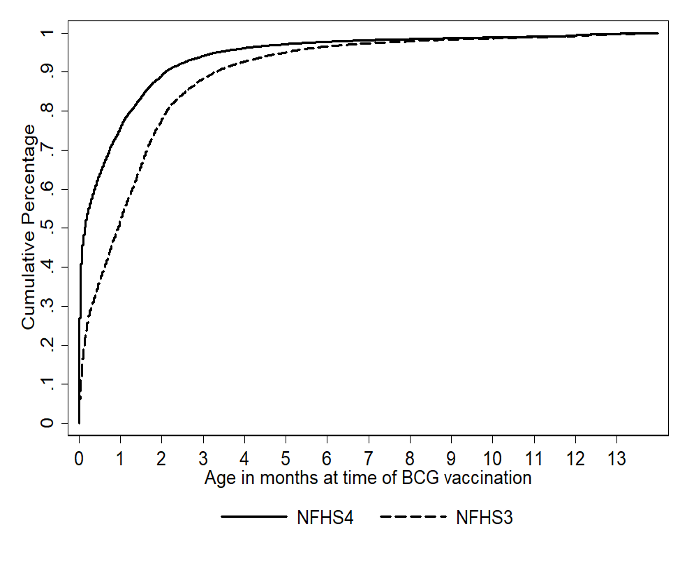
Figure 4. Change in timeliness of DPT-3/Pentavalent-3 for infants
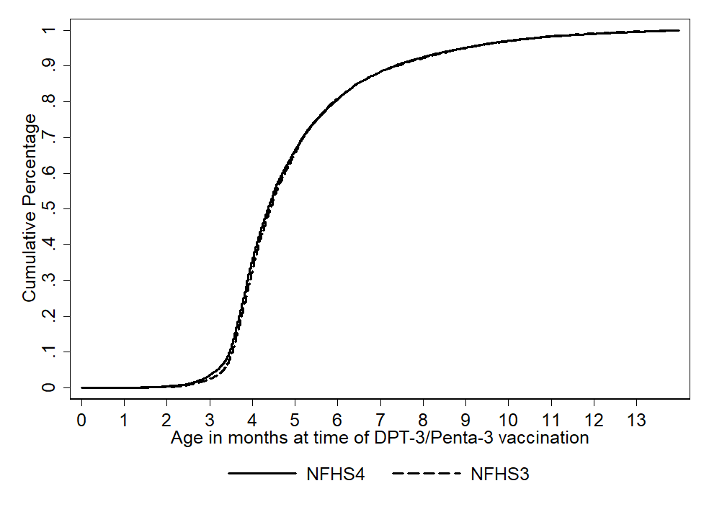
Figure 3 indicates that timeliness has considerably improved for BCG between the last two rounds of the NFHS Survey. This may partly be attributed to the significant increase in institutional deliveries from 24% in NFHS-3 to 54% in NFHS-4 (Mishra and Syamala 2021). In the case of DPT-3 in Figure 4, there was no perceptible change between the two rounds.
Implications of COVID-19
After the first COVID-19 induced lockdown in India in 2020, several reports indicated a disruption of routine health services. The Ministry of Health and Family Welfare (MoHFW) and the Indian Association of Paediatrics were quick to issue guidelines on emergency immunisation protocols (MoHFW, 2020). Despite concerted efforts of the authorities, according to the NHM (National Health Mission)’s HMIS (Health Management Information System) data, about one million fewer BCG, almost 1.4 million fewer measles and Pentavalent-1 vaccines, and 606,000 fewer OPV-0 vaccines were administered in April 2020 as compared to January 2020. The engagement of ASHA and ANM workers – who are instrumental to primary rural healthcare – in the COVID-19 response could be one of the probable reasons for fewer vaccinations.
Measuring vaccine disruptions amidst COVID-19
In recent IGC research (Debnath and Deo 2021), we conducted pilot surveys in four blocks in the district of Muzaffarpur in Bihar in April 2021, covering frontline health workers and primary caregivers. The respondents included 22 ANMs, 100 ASHAs, and 200 primary caregivers. Through these surveys, we aimed to gather information about their broad socioeconomic characteristics, patterns of time use, interaction among frontline health workers, knowledge of vaccination timeliness and effectiveness, as well as information about mobile application usage for example, ANMOL (ANM Online).
To understand whether routine vaccinations were disrupted during the first wave of the pandemic we summarise the vaccine coverage and timeliness from our survey data in Table 3.
Table 3. Reported vaccine coverage and timeliness in Muzaffarpur
Note: (i) The age range of infants is 5-13 months. (ii) We consider a vaccine timely if it is administered within seven days of the due date. (ii) Infants between 6-12 months with a valid date of vaccination on the MCP card were considered for timeliness calculations.
On average, coverage is high for most of the vaccines and we see a similar cascading effect for booster doses as in the NFHS data but to a much lower magnitude. The low coverage of the measles vaccination can partly be attributed to the narrow age range in the sample. Even though the timeliness statistics resemble the numbers from NFHS-4, these are relatively low. This could be a manifestation of COVID-19 induced delays for routine vaccinations. [7]
Policy recommendations
Since we see that coverage and timeliness of vaccines are inadequate – besides birth doses – it may be fruitful to incentivise health workers to focus on these particular vaccinations and perhaps introduce marginal monetary benefits for ensuring timely administration. Increasing awareness of the importance of timely delivery of vaccines among caregivers and frontline health workers may reduce the delays.
There can also be a focus on catch-up campaigns, especially for measles, due to the potential for an outbreak even with a marginal reduction in herd immunity (Shet et al. 2021). A targetted approach should be used for groups with higher chances of delayed vaccinations when designing routine immunisation micro-plans in primary care settings (Choudhary et al. 2019). Decentralisation of planning and management can also help improve outcomes. Formulating strategies to increase the involvement of community healthcare workers in the implementation and development of vaccine programmes can be helpful since they are deployed to ensure complete and timely vaccinations (Prinja et al. 2010)
Systems should also be put in place for creating a comprehensive database on healthcare service utilisation, disaggregated at multiple levels, enabling real-time monitoring and intervention by policymakers.
Editor’s note: This article was published in collaboration with Ideas for India.
Further Reading
- Awofeso, Niyi, Anu Rammohan and Kazi Iqbal (2013), “Age-appropriate vaccination against measles and DPT-3 in India–closing the gaps”, BMC Public Health, 13(1): 1-7. Available here.
- Barman, Manash Pratim, Krishnajyoti Nath and Jiten Hazarika (2015), “Factors affecting timeliness of immunization coverage among children of Assam, India: A cross-sectional study”, Journal of Health Management, 17(3): 274-284.
- Black, Robert E et al. (2010), “Global, regional, and national causes of child mortality in 2008: a systematic analysis”, The Lancet, 375(9730): 1969-1987.
- Centers for Disease Control and Prevention (CDC) (2013), “Global Routine Vaccination Coverage-2012”, Morbidity and Mortality Weekly Report, 62(43): 858-861
- Centre for Operations Research and Training (CORT) (2007), ‘Assessment of ASHA and Janani Suraksha Yojana in Orissa’, Report.
- Cherian, Vinu, Narinder Kumar Saini and Arun Kumar Sharma (2019), “Assessment of timely immunization in an urbanized agglomeration of East Delhi, India”, International Journal of Community Medicine and Public Health, 6(3).
- Choudhary, Tarun Shankar et al. (2019), “Delayed vaccination and its predictors among children under 2 years in India: Insights from the national family health survey-4”, Vaccine, 37(17), 2331-2339. Available here.
- de Cantuária Tauil, Márcia, Ana Paula Sayuri Sato and Eliseu Alves Waldman (2016), “Factors associated with incomplete or delayed vaccination across countries: a systematic review”, Vaccine, 34(24), 2635-2643.
- Guerra, Fernando A (2007), “Delays in immunization have potentially serious health consequences”, Pediatric Drugs, 9(3): 143-148.
- Ministry of Health and Family Welfare (2020), ‘Immunization Services during and post COVID-19 Outbreak’, Report.
- Izurieta, HS, TA Kenyon, PM Strebel, AL Baughman, ST Shulman and M Wharton (1996), “Risk factors for pertussis in young infants during an outbreak in Chicago in 1993”, Clinical Infectious Diseases, 22(3): 503-507.
- Kiely, Marilou Kiely, Nicole Boulianne, Denis Talbot, Manale Ouakki, Maryse Guay, Monique Landry, Chantal Sauvageau and Gaston De Serres (2018), “Impact of vaccine delays at the 2, 4, 6 and 12-month visits on incomplete vaccination status by 24 months of age in Quebec, Canada”, BMC public health, 18(1): 1-15.
- Liu, Li et al. (2016) “Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals”, The Lancet, 388(10063): 3027-3035.
- Mathew, Joseph L (2012), “Inequity in childhood immunization in India: a systematic review”, Indian paediatrics, 49(3): 203-223
- Ministry of Health and Family Welfare (2017), ‘Monthly Village Health Nutrition Day - GUIDELINES FOR AWWs/ASHAs/ANMs/PRIs’.
- International Institute for Population Sciences (IIPS) and ICF International (2017), ‘National Family Health Survey (NFHS-4), 2015–16’, Report.
- O’Leary, Maureen et al. (2016), “Vaccination timing of low-birth-weight infants in rural Ghana: a population-based, prospective cohort study”, Bulletin of the World Health Organization, 94(6): 442-451. Available here.
- Pati, Susmita Pati, Kristen A Feemster, Zeinab Mohamad, Alex Fiks, Robert Grundmeier and Avital Cnaan (2011), “Maternal health literacy and late initiation of immunizations among an inner-city birth cohort”, Maternal and child health journal, 15(3): 386-394.
- Shankar Prinja, Madhu Gupta, Amarjeet Singh and Rajesh Kumar (2010), “Effectiveness of planning and management interventions for improving age-appropriate immunization in rural India”, Bulletin of the World Health Organization, 88: 97-103.
- S, Rukmini (2020), ‘COVID-19 Disrupted India’s Routine Health Services’, India Spend, 27 August.
- Shet, Anita, Baldeep Dhaliwal, Preetika Banerjee, Andrea DeLuca, Kelly Carr, Carl Britto, Rajeev Seth, Bakul Parekh, Gangasamudra V Basavaraj, Digant Shastri and Piyush Gupta (2021), “Childhood immunisations in India during the COVID-19 pandemic”, BMJ Paediatrics Open, 5(1): e001061.
- Soans, Santosh, Attila Mihalyi, Valerie Berlaimont, Shafi Kolhapure, Resham Dash and Ashish Agrawal (2021), “Vaccination in preterm and low birth weight infants in India”, Human Vaccines and Immunotherapeutics, 1-12.
- WHO (2020), ‘WHO vaccine-preventable diseases: monitoring system: 2020 global summary’.
[1] The 12 vaccine-preventable diseases are diphtheria, pertussis, tetanus, polio, measles, rubella, a severe form of childhood tuberculosis, hepatitis B, and meningitis and pneumonia caused by Haemophilus Influenzae Type-B.
[2] Basic vaccines include one dose of BCG (bacille Calmette-Guerin; tuberculosis) vaccine, three doses of DPT (diphtheria, pertussis (whooping cough), and tetanus) vaccine, three doses of the polio vaccine and one dose of measles vaccine. The National Health Mission’s vaccine schedule is available here.
[3] The World Health Organization defines herd immunity as “indirect protection from an infectious disease that happens when a population is immune either through vaccination or immunity developed through previous infection”
[4] Accredited social health activists (ASHAs) are community health workers instituted by the Ministry of Health and Family Welfare as part of the National Rural Health Mission.
[5] Pentavalent vaccines contain five antigens (diphtheria, whooping cough, tetanus, and hepatitis-B, and Haemophilus Influenzae Type-B and it was introduced around 2014 to replace the DPT vaccine. In some instances, these vaccines are used interchangeably.
[6] The Mother and Child Protection (MCP) Cards acts as the first point of contact between pregnant women and the healthcare system. It records the due dates for all healthcare services and the dates of delivery including antenatal care, postnatal care, and family planning. It includes a detailed section to maintain immunisation records along with date of receiving the vaccination.
[7] However, these should be interpreted with caution as we use the data only for 200 hundred infants. The data about infants comes from their primary caregivers who were surveyed.

