
Ramping up early detection of COVID-19 with limited resources: The role of pool testing
The ability to rapidly detect COVID-19 is central to saving lives and protecting livelihoods. However, testing equipment and associated kits are expensive and in short supply. As a result, many countries are not conducting anywhere near enough tests. Worse still, many individuals are spreading the virus unknowingly and undetected. The situation is particularly acute in sub-Saharan Africa and threatens to get worse as countries across the sub-region begin to ease restrictions imposed in the wake of the pandemic. There is an urgent need to consider innovative testing protocols to maximise testing with limited available test kits.
Many have compared the COVID-19 pandemic to an invasion of an invisible army that must be fought with the world’s entire arsenal. Perhaps this is the case, but we also need to be more strategic than usual. While we take on COVID-19, the traditional battles against extreme deprivation and diseases such as malaria rage on. Moreover, the fight against COVID-19 itself is likely to be drawn out. Each wave will have a toll on health systems, livelihoods, and the very ability to take on the next wave. In the absence of a magic bullet, such as a vaccine, there is the need to be strategic in identifying and deploying the most effective and sustainable weapons as we confront this invisible army.
Exploring more sustainable measures to contain the pandemic
The need to be strategic is particularly critical for sub-Saharan Africa. At the onset, there were dire predictions for the death toll from COVID-19 in the region. Those predictions were not unwarranted. For example, sub-Saharan Africa has an inadequate health sector, incapable of managing COVID-19 cases at a similar footing to the rest of the world. Whether in terms of the number of doctors, ventilators, personal protecting equipment, or simple test kits, sub-Saharan Africa comes up short. Similarly, the region had very little fiscal headroom even before the pandemic.
So far, the region has managed to escape the worst of the pandemic, but this is neither the time to be complacent nor declare victory. This is the time to explore more sustainable measures to contain the pandemic. As elsewhere, countries in sub-Saharan Africa have instituted measures hitherto unimaginable, from closures of places of worship and economic lockdowns to mandatory quarantines, in a bid to control the spread of COVID-19. These measures are not sustainable. Indeed, countries such as Ghana have already lifted the lockdown of their economies, acknowledging this fact. Against the advice of health experts, countries around the world are going ahead with plans to lift those unsustainable restrictions.
As these restrictions are rolled back, timely and large-scale testing have become more important than ever. Currently, though, sub-Saharan African countries are doing poorly on both fronts. The average country in the region is testing just about three out of every 1000 individuals, with South Africa, Ghana, and Rwanda leading the pack (Figure 1).
Figure 1: Total COVID-19 tests per thousand in sub-Saharan Africa
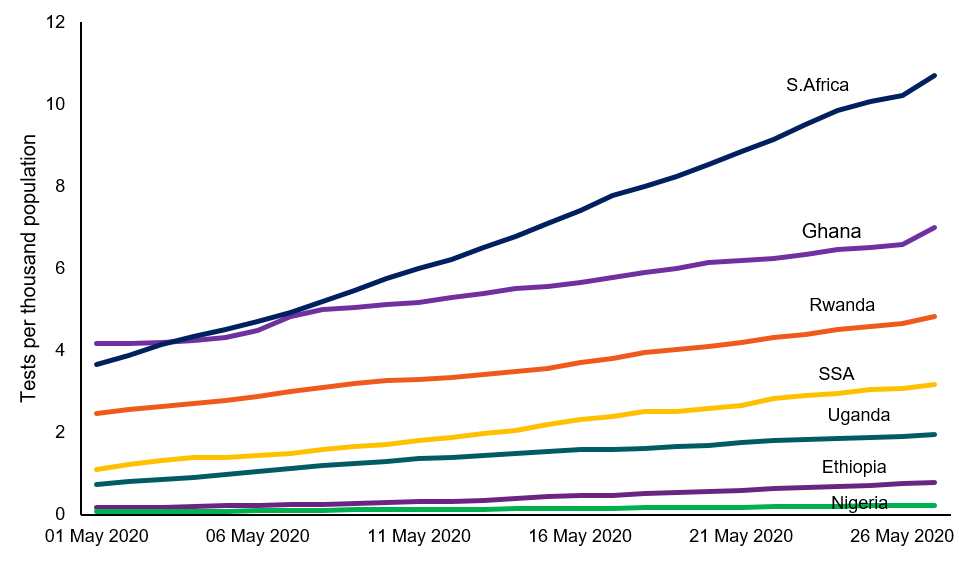 Data source: Our World in Data
Data source: Our World in Data
Nigeria and Ethiopia, Africa’s two most populous countries, are lagging way behind with less than one test per thousand of their respective populations. The inadequacy of tests are so acute in Nigeria that doctors have to “wait for three to five days for the tests results” of patients exhibiting COVID-19 symptoms. In a recent interview, Dr. Chikwe Ihekweazu, the Director General of the Nigerian Centre for Disease Control, attributed the backlog of tests to a scarcity of test kits globally. He went further to assure that Nigeria “… will be able to scale radically our testing capabilities” when the global test kit supply situation improves.
It has to be emphasised that this is not uniquely a Nigerian problem. There are far too many infected people spreading the virus unbeknown to them and the health authorities. How many exactly, nobody knows. What is known, however, is neither Nigeria nor the rest of the region can afford to wait until the global shortage of testing kits eases to ramp up testing. What is required urgently is a rethink of how to increase testing with the limited available test kits. In this regard, the Ghanaian pool testing experiment provides a useful starting point.
The Ghanaian COVID-19 testing regime
When the first batch of specimens came for testing, in early March, the Noguchi Memorial Institute for Medical Research (NMIMR) was the only facility capable of testing for COVID-19 in Ghana. Moreover, it had a very limited supply of test kits.
Faced with the harsh reality, scientists decided to exploit a standard testing methodology in which individual specimens are combined into pools and tested (Figure 2). When a pool tests positive, then each individual specimen of that particular pool is tested. The NMIMR started with a pool size of fives, which was later increased to ten as the testing needs and the understanding of test sensitivity parameters improved.
Figure 2: Test kit savings in a simple pool scenario
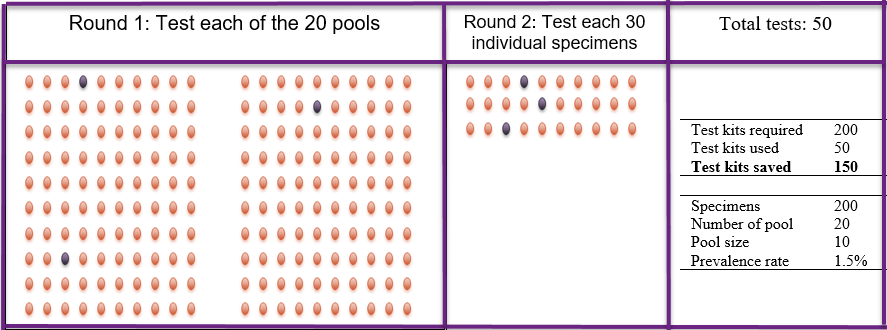
An important advantage of this version of pool testing is its simplicity. It requires no sophistication, and yet in a low prevalence environment, the savings on test kits is materially significant. Consider a test facility with a capacity of 200 tests per day. Assume the COVID-19 prevalence rate is 1.5%, as is currently the case in Ghana. Ordinarily, 200 test kits are needed. However, when 10 specimens each are combined into 20 separate pools, at most, 50 test kits are needed. In total, 20 kits are used to test each of the 20 pools, plus 30 kits to test the individual specimens in the three pools which test positive (Figure 2). That is a savings of 75%.
Keep it moderate, large pool sizes are not necessarily more efficient
A major limitation of the simple pool test protocol discussed above is that larger pool sizes do not necessarily save more test kits even at low prevalence rates (Figure 3).
Figure 3: Larger pool sizes do not save more test kits in simple pool test scenarios
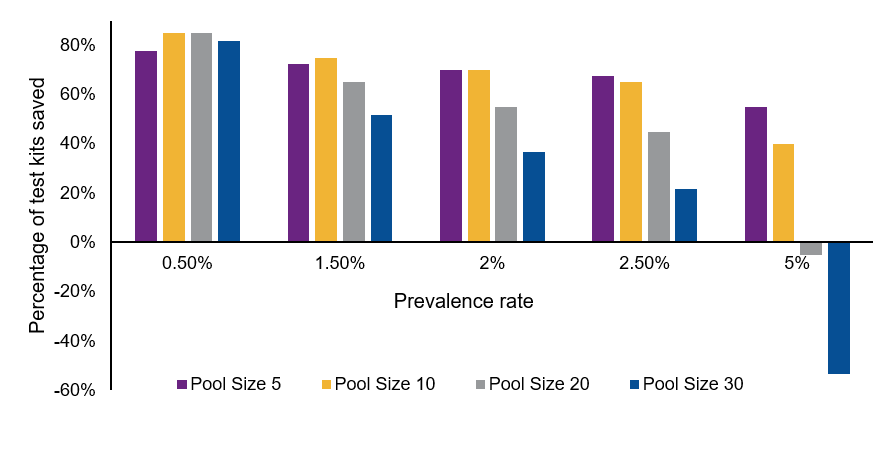
One recent study suggests a single positive specimen can be detected in a pool of up to 32 specimens, with an estimated false negative rate of 10%. However, even if policymakers tolerant a false negative rate of 10%, they may end up wasting rather than saving test kits. In the simple calibrations reported in Figure 3 above, a pool size of 10 specimens appears optimum in most cases. However, a pool size of 30 is least optimal, and in fact, increases the number of test kits used at prevalence rates of 5% and above. Hence, it is prudent to keep the pool size moderate in a simple pool testing regime.
Use differences in prevalence rates to save testing kits
In general, the gains from pool testing are reduced with the underlying prevalence rates. However, it is possible to exploit variations in the prevalence rate to increase the efficiency gains from pool testing. For example, instead of randomly pooling specimens, regional variations in prevalence rates within a country can be leveraged to save test kits.
This is particularly true for larger countries such as Ethiopia, Nigeria, and South Africa. Even in smaller countries, urban prevalence rates are much higher than in the countryside. Furthermore, within urban areas, such as Accra or Lagos, there are so-called hot spots. In these three examples, test kits could be conserved further when the specimens from less prevalence areas are pooled separately.
Furthermore, the likelihood of positive cases among individuals with COVID-19 related symptoms are higher than among the general population. It is therefore imperative to screen out the symptomatic cases and test them individually. The rest of the specimens can then be pooled and tested together.
Practitioners can push this further depending on country circumstances and the information available. For example, a number of countries are tracing persons who come into contact with people who test positive. Such specimens should not be pooled with specimens from the general population. This strategy of exploiting geographical, clinical, social, and any other available information can greatly save tests kits while reducing the risk of false negatives.
Increasing the sophistication of pool testing
The simple pool strategy involves only two test rounds. We can increase the rounds to save further on test kits. Horemheb-Rubio et al. (2017) provide an excellent schematic representation of a three-round split pool protocol (Figure 4).
Figure 4: Split pool testing
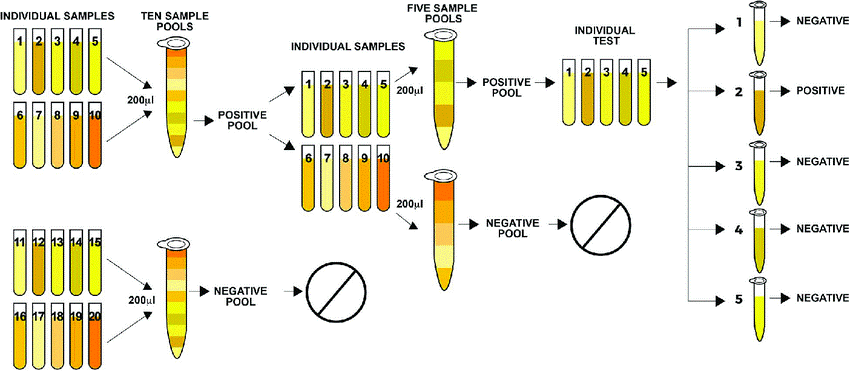
It involves pooling the specimens into equal sizes and then testing each pool, as before. In the second round, each pool that tests positive is split into two equal halves. The spilt pools are then tested. Finally, the individual specimens of a split pool are tested when the test result is positive. Figure 5 presents the results of a simple calibration demonstrating the potential efficiency gains from split-pool testing.
Figure 5: Efficiency gains from split pool testing vs. simple pool testing
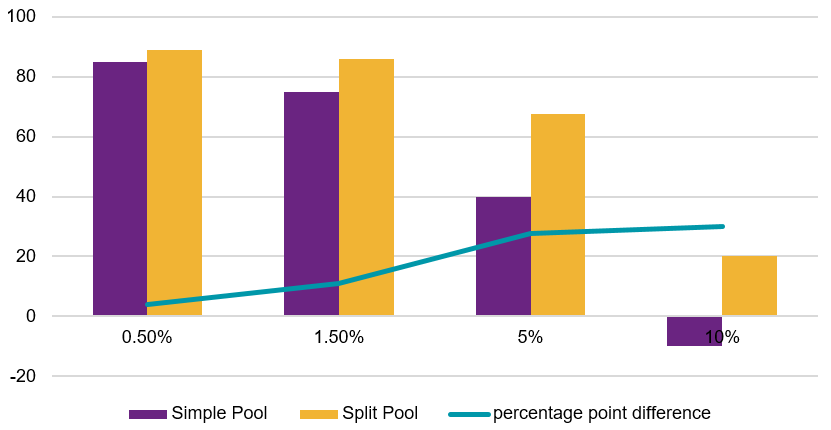
Two observations stand out. First, split pool testing saves more test kits for a wide range of prevalence rates. Second and most importantly, within a reasonable range, the extra gain from split pool testing increases with the prevalence rate. For example, at very low prevalence rates, the gains from simple and split pool testing are not significantly different. At a prevalence rate of 10%, where there are no gains from simple pool testing, split pool testing can still save a significant number of test kits.
Concluding remarks: Pool testing an important option, but with certain nuances
We have seen that most of the stringent restrictions imposed to contain the spread of COVID-19 are not sustainable. We have also seen that as those restrictions are lifted, the rate of infection threatens to pick up. The Ghanaian experience demonstrates that pool testing is an efficient tool to scale up testing even with limited resources.
There are three important implications for policymakers:
- Go beyond the simple pool testing. A split pool testing of just three rounds outperforms simple pool testing across a range prevalence rates.
- Keep the pool size moderate. The risk of false negatives increases with the pool size. Moreover, larger pool sizes do not necessarily save more test kits. It is therefore imperative to keep the pool sizes moderate.
- Leverage variations in prevalence rates. For each country, the prevalence rate varies across several dimensions. It is important to exploit the differences in the prevalence rates to save tests kits further while reducing the risk of false negatives.
References:
Horemheb-Rubio, G, P Ramos-Cervantes, H Arroyo Figueroa, S Avila-Rios, C Garcia-Morales, G Reyes-Teran, G Escobedo, G Estrada, T Garcia-Iglesias, N Munoz-Saucedo, D Kershenobich, P Ostrosky-Wegman and G Ruiz-Palacios (2017), “High HPgV replication with improved surrogate makers of HIV progression”, Plos One, 12(9).
Disclaimer: The views expressed in this post are those of the authors based on their experience and on prior research and do not necessarily reflect the views of the IGC.

